This trial focuses on children and young people with milk and peanut allergies in a ground-breaking £2.5m oral immunotherapy trial.
The study aims to plug the current Oral Immunotherapy (OIT) research gap by proving that everyday foods instead of expensive pharmaceutical drugs can be used as a practical treatment. If it's successful, our trial will empower the NHS to provide cost-effective treatments and the more cost effective they are, the greater opportunity to treat more people in the country with food allergies.
The study recruited 216 + people, aged 3 to 23, with one or more allergies to cow’s milk and peanut. Children will be aged 6 and above with a peanut allergy, and aged 3+ years for milk allergy. Each participant has been assessed to make sure they are suitable to take part in the trial. The six trial sites across the country are; Glasgow, Leicester, Sheffield, Newcastle, Imperial College London and Southampton. All the centres were responsible for recruitment.
Our study aims to prove that commonly-available peanut and milk products when taken under medical supervision, can be used as a treatment for people living with food allergies.
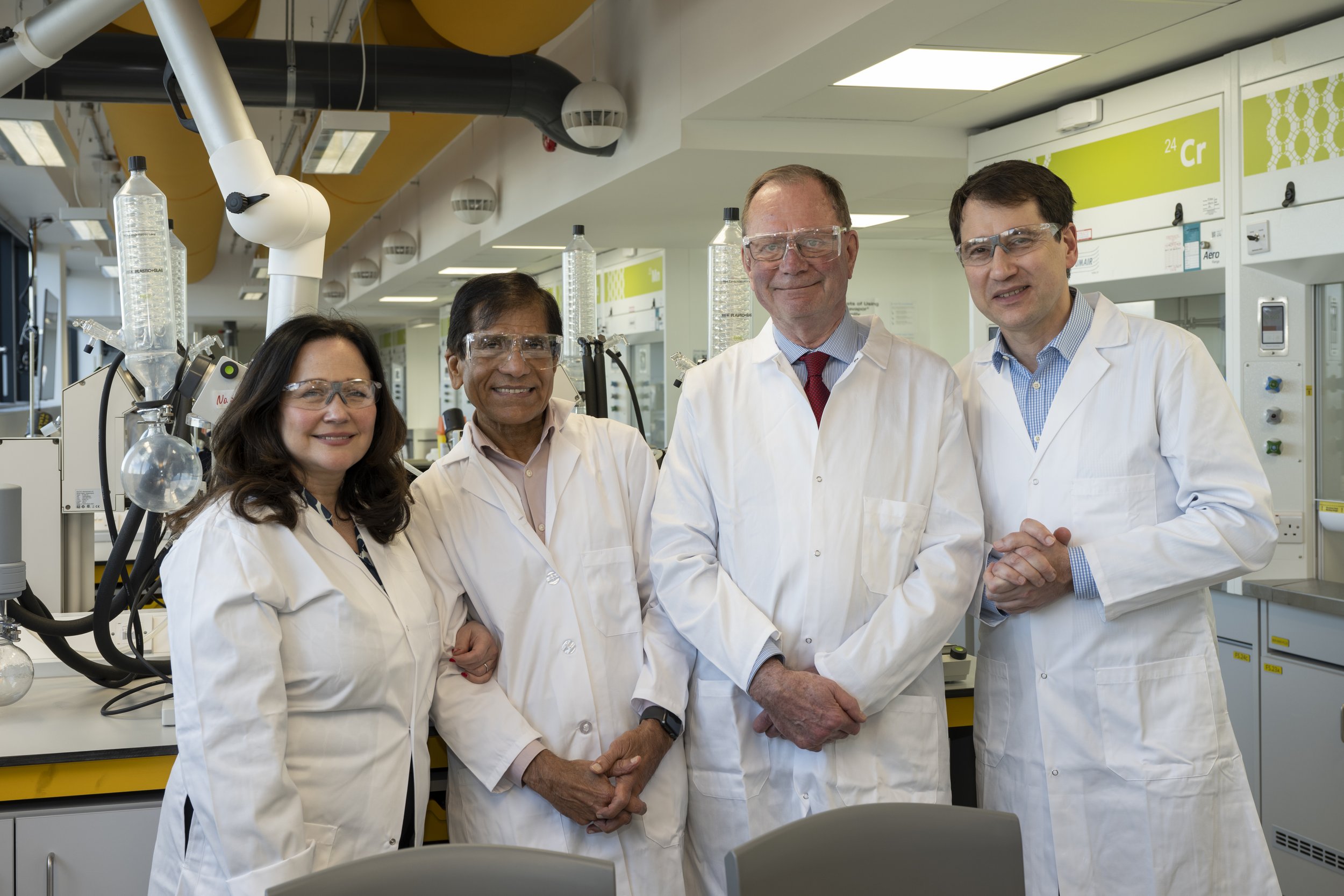
Founders of The Natasha Allergy Research Foundation -Nadim and Tanya Ednan-Laperouse OBE’s visiting the University of Southampton
This three-year oral immunotherapy (OIT) trial is the first major study funded by The Natasha Allergy Research Foundation, the charity set up by the parents of Natasha Ednan-Laperouse who died aged 15 from a severe food allergic reaction.
This Clinical Trial aims to show that everyday foods containing peanut or milk, which when taken carefully according to a standardised protocol under medical supervision, can be used as an alternative to expensive pharmaceutical drugs to desensitise patients.
If this trial is successful, participants with persistent food allergy will be able to live lives where they no longer have to avoid popular foods which might contain small amounts of allergens due to factory production lines or cross contact and also be able to eat popular foods like cakes, curries and pizza safely with their friends.
The £2.2m trial has been funded by a gift to the University of Southampton from The Natasha Allergy Research Foundation. Natasha's Foundation has received generous donations and funding, from its Clinical Trial Founding Partners. Fundraising and donations have also been received from Natasha’s Army of supporters.
The Clinical Trial Founding Partners are a consortium of food businesses: Greggs, Tesco, Just Eat, Co-op Morrisons, KFC, Bakkavor, Sainsbury’s, Bidfood, Costa Coffee, Elior UK, Burger King UK, Pret A Manger, Lidl, Leon, Cooplands and Uber Eats.
How Oral Immunotherapy (OIT) Changed 9-Year-Old Jamie’s Life
Watch this video to hear how Oral Immunotherapy (OIT) changed 9-year-old Jamie's life.
This trial is led by a team of Researchers at the University of Southampton partnering with Imperial College London (both World Allergy Organisation Centres of Excellence) together with University Hospitals of Leicester NHS Trust, Newcastle University and Sheffield Children’s Hospital. That’s a total of five big centres from the north to the south of our country.
In December 2020, NHS England announced the availability of Palforzia - a Nestlé-owned branded immunotherapy treatment for peanut taken daily for at least 2 years to treat children with peanut allergy.
In contrast, our first ‘NATASHA Trial’ will use ‘everyday foods’ instead of expensive pharmaceuticals for OIT. This could open up potential life-long treatment for millions of people worldwide living with allergies, at a fraction of the cost, and also affordable for our own precious NHS.
The study recruited a total of 216 + people between the ages of 3 and 23 with food allergy to cow’s milk and aged 6 and 23 with food allergy to peanut. Following an initial 12 months of desensitisation (carried out according to a standardised protocol under strict medical supervision), participants are monitored for a further two years in order to report on longer-term safety and cost-effectiveness.
The aim is to bring the level of evidence to a point where OIT can be used commercially-available foods could be approved for use in the NHS to treat food-allergic patients most at risk of anaphylaxis.
Natasha’s parents Nadim and Tanya Ednan-Laperouse, (pictured left) were both awarded OBEs this year for their services to charity and people living with allergies.
Tanya said:
“We have been determined that Natasha’s death should not be in vain. Following the successful implementation of Natasha’s Law, which has brought new ingredient and allergen labelling, we are delighted to announced this huge project which is very close to our hearts, the first NATASHA Trial.”
Nadim said:
“This is a major first-step in our mission to ‘make food allergies history’. The aim is to save lives and prevent serious hospitalisations by offering lifelong protection against severe allergic reactions to eventually any number of foods or ingredients. The study aims to plug the current oral immunotherapy research gap by proving that ‘everyday foods’ rather than pharmaceutical drugs can be used as a practical treatment for children and young adults with allergies.
If successful, this will empower the NHS to provide cost-effective treatments for people living with food allergies through oral immunotherapy.
It would enable people, once desensitised under clinical supervision, to control their own lives and stay allergy safe using shop bought foods rather than relying on expensive pharmaceutical products”.
Professor Hasan Arshad, Professor of Allergy and Clinical Immunology at the University of Southampton, said:
“This project presents a unique opportunity to establish immunotherapy as a practical treatment that will allow people with food allergies to live a normal life. I am immensely proud that the University of Southampton will be leading this trial in collaboration with an elite group of partner universities and clinical allergy centres.”
Co-chief investigator is Dr Paul Turner, Reader in Paediatric Allergy & Clinical Immunology at Imperial College London said:
“This study heralds a new-era for the active treatment of food allergy. For too long, we have told people just to avoid the food they are allergic to – that is not a treatment, and food-allergic people and their families deserve better.”
Q. What is food immunotherapy?
A. Immunotherapy is a medical treatment that uses the body’s own immune system to fight disease outcomes. When used to treat food allergies, it involves giving the patient, under medical supervision, tiny but increasing amounts of the food to which they are allergic. This gradually trains the immune system not to see the food as a threat, triggering an allergic reaction. When the food is given by mouth, this is known as oral immunotherapy or OIT. Successful OIT was first reported in a 13-year-old boy with egg allergy in 1908 in the medical journal The Lancet. However, it is only in the last 15 years that trials have been carried out showing that OIT can work in up to 80% of patients with allergies to cow’s milk and peanut. Despite these impressive results, OIT is still not widely available on the NHS.
Q. How could the Natasha Trial help people with food allergies?
A. Currently, the main strategy for the 2 to 3 million people living with food allergies in the UK is avoidance of the food they react to, and in many cases, prescribing adrenaline autoinjectors if they are at risk of anaphylaxis. However, trying to avoid the food to which you are allergic can be difficult, especially when eating out. Even when following good avoidance, typically someone with peanut allergy has an accidental reaction once every 2-3 years , often due to undeclared contaminants.
OIT offers the possibility of a long-term solution – once the body has been desensitized to the food, food-allergic individuals no longer need to worry about small amounts of accidental allergen presence. However, they must carry on eating a specific amount of the allergen in order to maintain the desensitization effect. The trial will achieve this by using “everyday foods” to keep up this level of tolerance. The aim of the trial is to establish OIT as a practical treatment for food allergy to allow people to live a more normal life.
Q. Which food allergies will be included in the trial?
A. The trial will look at OIT for two foods: peanut and cow’s milk.
Q. Is oral immunotherapy an expensive treatment?
A. OIT needs to be carried out under the supervision of a trained specialist. However, as the treatment uses everyday foods rather than a pharmaceutical pill, the cost of the treatment itself is very cheap. That is the beauty of the trial. We hope it will provide cheap, accessible solutions that the NHS can offer for people with food allergies.
Q. Is it a cure?
A. No. Studies have shown that OIT is around 80 per cent successful in treating milk and peanut allergies. This means that eight out of 10 people who have the treatment, will respond to it. However, for the treatment to remain successful, in most cases patients must continue to consume the food regularly or the desensitisation will be lost. We hope to run a follow-on study to continue to monitor participants after 3 years, to see if longer term desensitisation is achievable without them needing to continue to eat small amounts of the food on an ongoing basis.
Q. How is this trial different from other food immunotherapy trials?
A. Many trials have already proven that OIT is an effective treatment for peanut, cow’s milk and particularly in young children. What this trial hopes to do is come up with the evidence that OIT is safe and cost effective and improves people’s quality of life so that it can be widely introduced on the NHS. The NATASHA Trial will also look at teenagers and adults, as well as younger children. This is different from other trials, many of which have tended to focus on younger children.
Q. Why is this trial needed?
A. Despite previous trial results showing it is effective, OIT has not been widely approved by the National Institute for Health and Care Excellence (NICE) for use in the NHS. This study will plug the research gap by hopefully proving that everyday foods can be used as a practical treatment for children and adults with allergies. The Natasha Trial is a gold-standard medical trial known as a randomised-controlled trial. That means some patients will receive the OIT treatment, and other won’t. This gives the researchers the best possible information to prove that OIT can be cost-effective compared to standard care (avoiding the allergen), and provide the NHS with the information needed to make this treatment more widely available to people living with food allergies. The control group will get the chance to have OIT after two years.
Q. What about the peanut immunotherapy pill Palforzia?
A: In February 2022, the National Institute for Health and Care Excellence (NICE) approved the use of Palforzia for treating peanut allergy in children aged 4 to 17 (this can be continued in people who turn 18 while on the treatment). This pharmaceutical product, a powder manufactured from peanuts, is designed to be used for OIT for peanut allergy, potentially reducing the severity of any allergic reactions. In studies, around half of people taking Palforzia were able to tolerate at least 1000mg peanut protein, compared with just 2 per cent who were not taking the drug. The cost of a year’s treatment with Palforzia is estimated to be around £10,000 (£3700 for the medicine, with additional costs for hospital visits every 2 weeks during updosing and support costs). Using a combination of “real-world” everyday foods together with telemedicine would offer a cheaper and significantly more accessible alternative to Palforzia, is likely to improve the quality of life for people with allergic disease, and also opens up the possibility of using this approach for food allergies other than peanut.
Q. Can I join the study?
A. The study is recruiting 216 people, aged 3 to 23, with one or more allergies to cow’s milk and peanut. Children must be aged 6 and above with a peanut allergy, and aged 3+ years for milk allergy. Each participant will be assessed to make sure they are suitable to take part in the trial. The five trial sites across the country are; Leicester, Sheffield, Newcastle, Imperial College London and Southampton. Initially, these centres will be responsible for recruitment.
Q. How long is the study?
A. The study is expected to run for three years.
Q. How will participants on the study be treated?
A. Participants will be randomly allocated by computer to either receive the OIT treatment or standard care (food avoidance and adrenalin autoinjector) for the first 2 years. Patients allocated to OIT will be given tiny amounts of the food by mouth to which they are allergic, according to a standardised protocol under medical supervision. This amount will then be increased little by little over the year, either in a clinic or at home. Participants and families will also have access to a 24-hour helpline. If the OIT is successful, the participant will be given detailed advice about which everyday foods they can buy from shops and how much they should eat at home to maintain their tolerance. They will be monitored for another year. The control group will get the chance to have OIT after two years.
Q. Is it safe?
A. All medical treatments carry risks and OIT is no exception. There is a risk that the patient will have an allergic reaction to the very small amounts of food they are given which is why OIT must be carried out under medical supervision. However, previous studies suggest it works for around 80 per cent of people. The trial is not suitable for people with uncontrolled asthma, atopic dermatitis, severe allergic rhinitis, other severe and chronic diseases, and pregnant women. Robust safety protocols are in place for the NATASHA Trial, including a 24 hour helpline.
Q. When will the results be published and what will they show?
A. The study is due to finish in 2025 and the results will be published once the findings have been analysed. The researchers will measure a range of factors including whether OIT is effective, improves the patient’s quality of life and whether the treatment is cost-effective.
Q. How will these results help the wider food allergy community?
A. The results of this trial should provide irrefutable evidence that OIT can work in the NHS setting, transforming the way people living with food allergies are treated and offering them a practical solution to allow them to live a more normal life. This will improve the quality of life for people living with food allergies and significantly reduce the need to avoid the foods they are allergic to. If successful, the trial results will be the first to examine longer-term cost-effectiveness and safety, and will be used to support the case for OIT to be made widely available on the NHS. OIT empowers people at risk of anaphylaxis to food to take control of their own lives and stay allergy safe using shop-bought foods rather than expensive pharmaceutical products. It will also deliver the first win in the Natasha Foundation’s mission to Make Allergy History.